Osto-Mate
Interactive Training Model for Colostomy Care in Low Resource Settings
in collaboration with christine luk, elisa arango, jennifer lee, dr. kathleen schmeler
Problem Statement
Colostomy surgeries are sometimes necessary to treat various forms of diseases and cancers near the pelvic and intestinal areas. Although life-saving, colostomy procedures have a significant effect on quality of life. After surgery, patients wear colostomy bags in order to collect intestinal waste. Patients often encounter physical, psychological, and social problems as well as initial difficulties in their daily lives. Both quality of life and ease of adaptability for users are improved significantly through improving confidence in managing their colostomy bags. Currently, only 10% of patients show a high confidence in ostomy bag management within a year of receiving stoma surgery in the US. Most patients are provided with care pamphlets or instructional videos and have limited or no access to hands-on ostomy bag care instruction. The current state of self-care training for patients is lacking especially in low- and mid- resource settings and often results in low user confidence.
Though forms of interactive physical training models do exist, they are rarely used due to lack patient availability in mid and low-resource settings. Current training models also do not provide live feedback for positive and negative reinforcement on patient actions. An affordable and interactive training model would enable more patients the opportunity to observe and practice proper colostomy bag care techniques before their surgery, thus expediting the learning process. The model will ideally simulate proper application, maintenance, and disposal of the colostomy bag and incorporate common real-life complications such as bag leakages and bleeding from the stoma. The design will focus on usability in low- and mid- resource settings.
Work Done and Proposed Solution
The design of the training model began with a literature review of the current state of colostomy care and patient training and the best practices in colostomy bag management. From the information learned, design criteria were developed as listed below:
- Impact on retention and confidence
- Ease of use
- Minimize cost
- Durability
- Accuracy of feedback indicators
With the idea for a smaller and interactive model in mind, the training elements of the model include:
- Bag application and stoma sizing
- Stoma discharge
- Bag cleaning and disposal
- Skin care
- Stoma complications
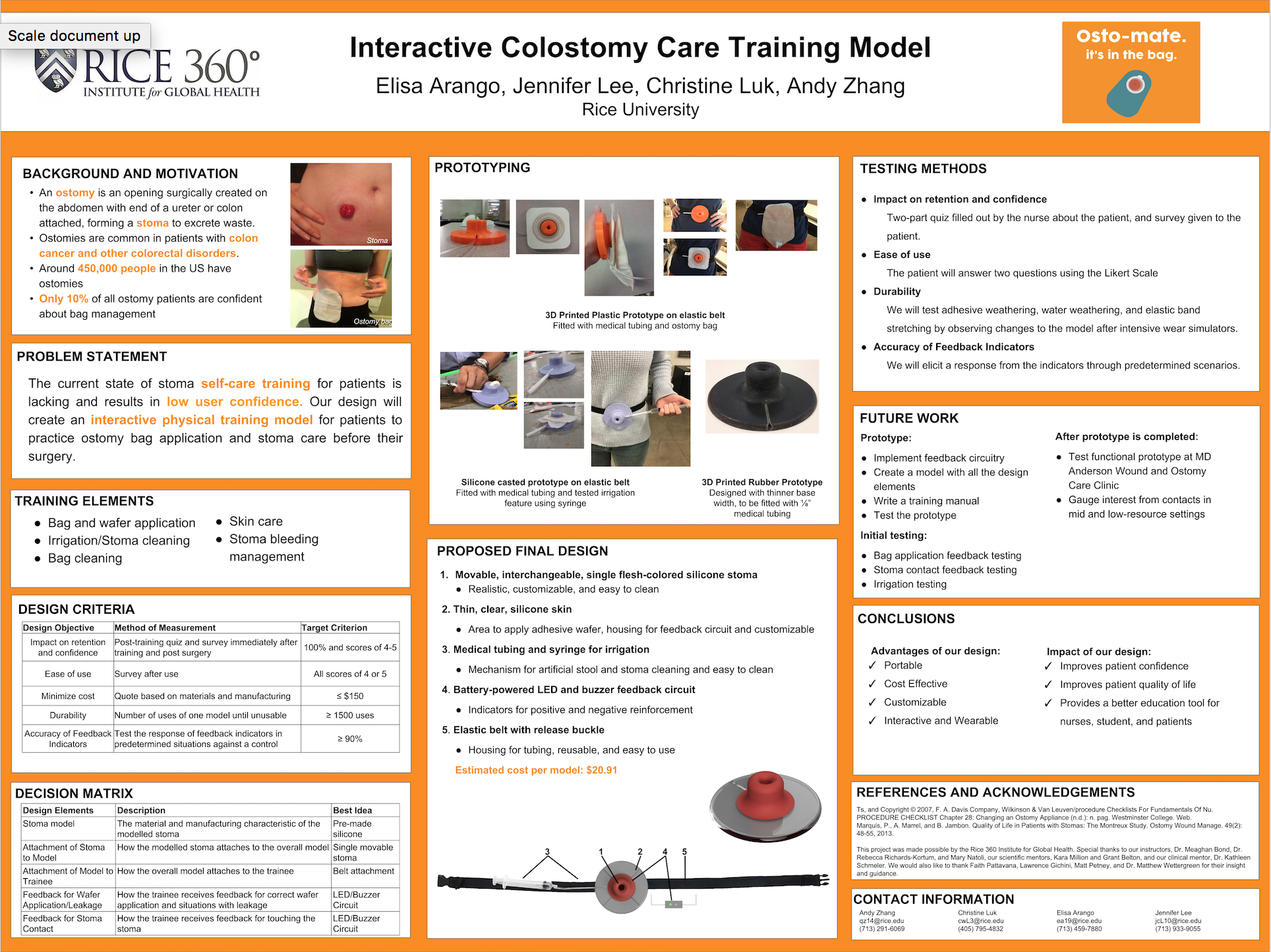
The initial designs were sketched on paper and labeled with features that met the training goals of the model as shown (Figure 1 and 2). These features include transparent silicone to mimic the texture and color of skin and to allow for skin care practice, an elastic band with a release buckle to attach to the body as movable model, medical tubing with a syringe to mimic stoma discharge and cleaning, and a feedback mechanism for bag application and stoma sizing practice.
The initial prototypes were low-fidelity and were made out of Play-Doh, clothespins, fabric, and velcro (Figure 3). The low fidelity prototypes acted as proof on concepts to show that there are benefits to having a movable single stoma model and that the best practices for training could be performed.
Figure 1. Drawing of the main components
Figure 2. Drawing of bag interface
Figure 3. Initial low-fidelity prototype
After evaluating the proof of concept prototypes, a 3D model was created on Fusion 360 CAD software (Figures 4 and 5). This model allows for planned dimensions to be visualized and for a more realistic representation of various features coming together as the materials and colors can be adjusted.
Figure 4. Isometric view of 3D model
Figure 5. Front view of 3D model
The model was converted to a stereolithography (STL) file for 3D printing with ABS plastic. The purpose of the print was to create a quick prototype for visualization of our envisioned model (Figure 6). The print allowed us to find that our initial dimensions produced too thick off a base plate or skin layer, not enough fillet for realistic curvatures, too large of a stoma, and too small of an opening for medical tubing. The print also allowed us to create a negative mold to start developing silicone prototypes, which was the original goal material. The silicone prototypes allowed us to understand the texture and the material properties of silicone as a model material. Silicone also allowed us to reevaluate the practicality of the dimensions with an elastic material and to test the use of medical tubing and a syringe to mimic discharge from a stoma (Figures 7 and 8). After various iterations, we determined that silicone manufacturing with our negative mold was not feasible as there were too many imperfections causing air pockets to form and too many restrictions on the geometries we could design.
Figure 6. 3D printed ABS prototype
Figure 7. Silicone molded prototype
Figure 8. Silicone molded prototype
Figure 9. Locking mechanism of 3D printed rubber prototype
Ultimately, the final prototype was 3D printed, but with Tango Black rubber material. This method of manufacturing allowed for similar textures as the silicone with much higher precision. 3D printing the training model also allowed for the addition of the desired feature of adjusting the size and shape of the stoma. A unique and innovative mating and locking mechanism was designed to allow for the stoma part of the model to be switched out while the rest of the model stayed the same (Figure 9). The mechanism was designed with the geometric capabilities of 3D printing in mind.
The feedback indicator works by lighting up an LED through the completion of an open circuit attached to the colostomy bag by a conductive contact ring on the training model itself (Figure 10 and 11). The feedback indicator mechanism is important in signaling a successful colostomy bag sizing and application to positively reinforce correct practice and to improve confidence levels.
Figure 10. Feedback indicator mechanism of final prototype
Figure 11. Feedback indicator mechanism and overall final prototype
The features of the final prototype include:
- TangoBlack material (Rubber-like) for mimicking stoma and skin
- Single stoma model for realism and lower cost
- Interchangeable parts to account for variation between patients
- Attachable to body for realism
- Feedback indicator for colostomy bag application/wafer sizing (attachable to any bag)
- Discharge tubing traveling from stoma opening out of skin layer
The demonstration of the functional prototype of the interactive training model for colostomy care is shown in the video below. A training guide for a deeper understanding of the training model and troubleshooting information and a product information sheet are also available for the product.
The final prototype is an interactive training model for colostomy care. With user-centered design principles guiding its development, the training model can be used across all educational backgrounds and will improve both comfort and confidence in colostomy care and management, which will in turn improve overall quality of life.
Outcome and Future Work
Results from initial testing showed that users have an average confidence rating of 4.6 out of 5 and that the training model is durable for at least a full years worth of use after 48 cycles of adhesive weathering, liquid weathering, and stretching. Results also showed that the feedback indicator has perfect accuracy and precision. The functional prototype of the interactive training model for colostomy care along with its supplementary documents were taken abroad to global health partners in Malawi and Brazil for initial use testing in low-resource settings. After three months of demonstration in Brazil, the training model is now under consideration for clinical studies by colorectal surgery teams at the Federal University of Goiás and the University of São Paulo.
After clinical studies, work will be done in optimizing the design for mass manufacturing and distribution and in improving its functionality and usability. Manufacturing of the model will switch from 3D printing to injection molding in order to reduce costs. The size of feedback indicator housing will be reduced to decrease bulkiness and the battery changing mechanism for the feedback indicator will be improved for ease of use. To improve the aesthetics of the training model, the contact ring will be embedded and a smoother path for the irrigation tubing will be made. Additionally, new prototypes with transparent skin layers will be created to match the patient's skin and different sized and shaped stomas will be created to mimic those that are less ideal.